|
Let me start with a provacative question: How serious is COVID-19? Clearly it is deadly, and you need look no further than the constant headlines of the NYT, follow just about anyone on Twitter, own a Facebook account, or just basically not live under a rock (Maybe your safest place currently). But, we have a really really hard time right now understanding the magnitude of this. It really shouldn't be quite this hard though- we need to make some short-term tradeoffs for a clearer understanding of long-term tradeoffs.
I propose two ideas, both involving random samples of the population. First, we randomly sample ~1K to ~10K individuals to receive tests. We may need to provide incentives to these individuals. We need as much participation as is possible. Because, those who are less likely to do it may have behaviors that are different than those who do and related to being positive. We need to track everyone we asked to participate. This will give us a better sense of the true percentage of the population that are currently affected. Maybe better, Abbott Labs has apparently just produced an antibody test that would allow us to know who is immune as a result of already having it. Of course, there is some percentage of the population that had it and perished because we didn't test early enough; however, if we did a comparable random sample we could track the sub-sample that did not have it over time and see what happens as we re-open the economy. We would also have a sense of how many in society currently have it- by the way we may be able to use their blood to help others recover. Given that 25%-60% of individuals may be "silent carriers" an Economist article suggests the infection rate may be 200X what we think it is. In the US, this could mean more than a 1/3rd of the population has already had it. That would actually be wonderfully welcoming news (Like very seriously some of the best news you have heard since this started) because it means that most of us are immune and a really large percentage of us are asympotomatic and it won't be fatal. This doesn't mean to go out now and celebrate- we can still overwhelm our health care system and many will die who would otherwise survive. Our elderly will still be at great risk, and we can still protect them through smart policies. We don't know if the economist article is right, but I believe we would have a much better understanding of whether this is the case if we randomly test about 10K individuals across the US with these Abbott tests. Even now, that would be taking one days worth of tests or less and using it to this end.
0 Comments
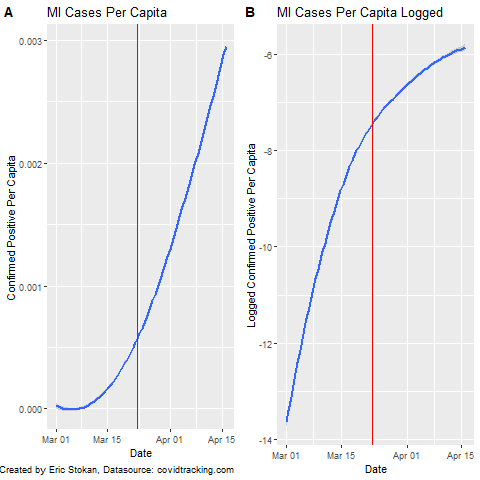
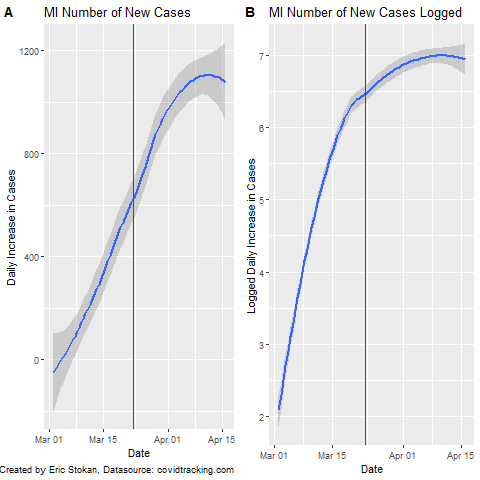
You will notice that most of the charts I have produced rely on a linear scale; however, some like @JamieFlournoy suggested that displaying it this way is problematic as using a log scale should be better. This has recently been elaborated upon by Sevi et al. (Forthcoming) in the Canadian Journal of Political Science (Manuscript here). So, I decided to just quickly display both types of plots here as the Sevi et al. article makes clear that we perceive these very different despite them providing the exact same information simply scaled differently. As a note, the red line represents when MI put their "stay at home order" in place. Going forward, I will be analyzing state policies to determine how policy responses have impacted important COVID-19 related outcome measures. Because expressing these data in per capita terms provides a scale that is not as easily interpretable, I also provide the number of daily cases (new) in MI and the logged number of new cases. In actuality, we know that testing rates in MI are quite low right now relatively speaking - even the death toll is undercounted.
These different charts are simply meant to show how important the scale is when interpreting what the data display. We need to be even more careful regarding how we interpret the data and the limitations that exist. We continue to try and sort out the data and information coming in on COVID. At points it is a challenge to make sense of- but luckily groups like Data Driven Detroit are here to help. See their page on how to interpret much of this data.
If you are focused on incidence rates, I've been contributing to Drawing Detroit's analyses on the region. There are many decisions and assumptions that have to be made because of data quality, but we all need to identify those as best we can. One issue we all have right now is how to separate out new confirmed cases from the fact that testing rates are also increasing. A seemingly obvious way to do this though is to look at trends in newly confirmed cases as well as trends in deaths per confirmed case. When we have reporting on total tests (both positive and negative this is not as big of an issue). If these are truly new cases then the death toll should continue to increase with some lag; however, if this is a result of testing we should not see such an increase. This is a testable proposition and we can determine the lag from new confirmed case to death and use this to understand whether increases in testing are the primary driver of newly identified cases. The lack of testing has increased the death per confirmed cases in MI considerably according to Deadline Detroit. I have a recently published an article, with Aaron Deslatte at Indiana University Bloomington, at State and Local Government Review where we explored whether metropolitan areas that had higher levels of fragmentation (meaning more general purpose governments) that spanned more than one state (we coined this "Bordered fragmentation" to indicate its uniqueness from "horizontal" and "vertical" fragmentation) lead governments to utilize more economic development incentives. We found that to be the case, but it also mattered whether the government was run by a manager or a mayor. Finding mechanisms to mitigate these ultra-competitive environments would be beneficial to regions in addressing this misallocation of resources. You can find the article here if you are interested.
Also, one such anti-poaching arrangement in light of COVID is happening in one of the regions that spans multiple states metro-DC.development-leaders-in-six-counties-form-regional-alliance/ I will add more later, but here are some great new COVID resources:
First, Mathematica has helped to pull together some of the top resources and data sources for COVID: https://www.mathematica.org/features/covid-19-curated-data-modeling-and-policy-resources One source I am particularly interested in is the state-level response to COVID: https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/ A great snapshot of the data by country with recovery rates and fatality rates: https://ncov2019.live/data News and data based on your personal location: https://topic.newsbreak.com/covid-19.html COVIDNearYou is pretty interesting as people self-report, which is great since testing has been slow and backlogged: https://covidnearyou.org/#!/#top I have begun tracking a much wider array of statistics on Coronavirus and will be updating the blog more frequently, but here are some numbers out of Metro-Detroit which turns out to be one of the hotspots for COVID cases and deaths sadly. In future blogs, I hope to integrate data from FlightRadar24 which shows how many flights are still coming into Metro-Detroit from all over the world. In this post, I calculate the most recent statistics for Metro-Detroit. Here we see the number of confirmed cases by County. The problem with this of course is that the raw number does not tell us anything about the population size, so I standardize by population. The next visual shows the cases in per capita terms. I notice that the number of cases in per capita terms is still a fraction of 1% of the population. We are of course worried about the fatality rate. So, I look at the percentage of confirmed cases that result in death. But, I am interested in seeing the relationship with population density. I want to do this on a broader scale, but for now focus on metro-Detroit in tabular form. I intend to run correlations when there are enough counties to establish this relationship. I am still very suspect of the data, in this case Monroe County is reporting no deaths but this is likely a statistical improbability based on the number of confirmed cases. In the table above, from April 7th, we see that the number of confirmed cases that result in death varies considerably (18.2 to 77.5); however, there clearly seems to be a relationship between this proportion and population density. Yet, we also know that density is associated with many other demographic factors and to appropriately analyze these relationships we need a larger data set and to control for many other factors. This will form the basis of future analyses.
|
Eric StokanI am an assistant professor of political science at the University of Maryland Baltimore County (UMBC). I completed my Ph.D. in Public Policy and Public Administration at George Washington University. Archives
February 2022
Categories |



 RSS Feed
RSS Feed